The vagus nerve has long been recognized as a critical pathway in the body's intricate communication network, but recent discoveries have unveiled its role as a master regulator in the gut-brain axis. This bidirectional superhighway not only transmits signals between the digestive tract and the central nervous system but also appears to hold the key to understanding inflammatory responses. Scientists are now decoding what some call the "vagus neural cipher"—a complex language of electrical and biochemical signals that may revolutionize how we treat chronic inflammation.
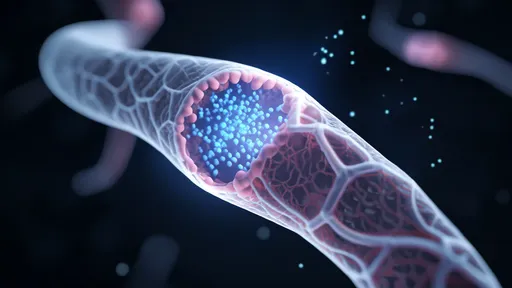
At the heart of this discovery lies the inflammatory reflex, a neural circuit that detects and modulates immune activity. When inflammation occurs in the gut, specialized receptors called nociceptors activate the vagus nerve, sending distress signals to the brain. In response, the brain sends return signals through the vagus that can suppress excessive inflammation. This closed-loop system functions with remarkable precision, like a biological feedback system constantly fine-tuning our immune responses.
The implications of this neural dialogue extend far beyond basic physiology. Researchers have identified specific patterns in vagus nerve signaling that correlate with various inflammatory bowel diseases. These patterns appear to follow a discernible code—different firing frequencies and durations correspond to specific inflammatory states. By deciphering this code, scientists aim to develop targeted neuromodulation therapies that could potentially reset dysfunctional inflammatory responses in conditions like Crohn's disease and ulcerative colitis.
What makes this discovery particularly groundbreaking is the realization that the vagus nerve doesn't merely transmit information—it processes it. The nerve contains intrinsic ganglia that can make local decisions about inflammatory regulation without always requiring input from the brain. This distributed processing capability suggests the gut-brain axis operates more like a neural network than a simple communication line, with the vagus nerve serving as both conduit and processor.
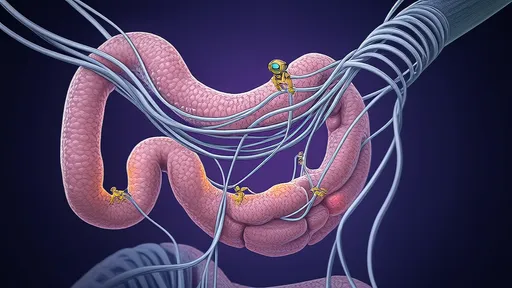
Clinical applications of this research are already emerging. Vagus nerve stimulation devices, originally developed for epilepsy treatment, are showing promise in managing inflammatory conditions. Early trials demonstrate that precisely timed electrical pulses can mimic the body's natural anti-inflammatory signals, reducing symptoms in patients with rheumatoid arthritis and other autoimmune disorders. The challenge lies in refining these stimulation parameters to match the body's own neural code for inflammation control.
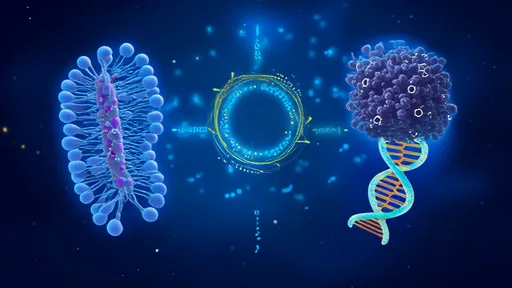
The gut microbiome plays a crucial role in this neural-inflammatory dialogue. Certain gut bacteria produce neurotransmitters and metabolites that directly influence vagus nerve signaling. This microbial-neural cross-talk creates a three-way communication system where bacteria can effectively "speak" to the brain through the vagus nerve, potentially modulating inflammatory responses. Disruptions in this microbial community may contribute to the breakdown of normal inflammatory regulation, leading to chronic conditions.
Understanding the vagus nerve's cryptographic-like signaling system opens new possibilities for treating systemic inflammation. Unlike traditional anti-inflammatory drugs that work through biochemical pathways, neuromodulation approaches target the neural control systems that govern these pathways. This paradigm shift could lead to treatments with fewer side effects and more precise control over localized versus systemic inflammation.
The therapeutic potential extends to neurological conditions with inflammatory components. Emerging evidence suggests that dysfunctional gut-brain communication may contribute to neuroinflammatory processes seen in depression, Parkinson's disease, and even Alzheimer's. By restoring proper vagal tone and signaling patterns, researchers hope to develop interventions that address both gastrointestinal and neurological symptoms simultaneously.
As research progresses, scientists are mapping the "vagus neural cipher" with increasing resolution. Advanced imaging and electrophysiological techniques allow researchers to observe real-time signaling patterns in unprecedented detail. Machine learning algorithms are being employed to identify subtle patterns in these complex neural signals that human researchers might miss. This combination of neuroscience and artificial intelligence may soon crack the complete code of vagus-mediated inflammatory regulation.
The closed-loop nature of this system presents both challenges and opportunities for therapeutic development. Unlike open-loop systems where inputs and outputs follow a linear path, the gut-brain axis operates through continuous feedback. Effective interventions will need to account for this dynamic interplay, potentially requiring adaptive devices that can respond to changing physiological conditions in real time.
Future directions in this field point toward personalized neuromodulation therapies. Just as genetic testing has enabled precision medicine, decoding an individual's vagus neural patterns may allow for customized stimulation protocols. This approach could optimize treatment efficacy while minimizing side effects, representing a significant advancement over current one-size-fits-all approaches to managing inflammation.
The exploration of the vagus nerve's role in inflammatory regulation represents a convergence of neuroscience, immunology, and gastroenterology. As we continue to decipher the complex language of the gut-brain axis, we move closer to a new era of medicine where neural modulation becomes a primary tool for managing chronic inflammation. The implications for patient care are profound, offering hope for millions suffering from inflammatory conditions that have proven difficult to treat with conventional approaches.

By /Aug 14, 2025
By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025

By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025

By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025
By /Aug 14, 2025